Health anxiety is a real thing. It refers to when someone spends an excessive amount of time worrying about their health, whether it’s fearing they are ill, potentially fatally, or dreading the possibility of falling ill in the future. This constant worrying about health can significantly reduce a person’s overall quality of life.
I have what I call, healthCARE anxiety, although it doesn’t seem to be a thing. Some people with health anxiety avoid seeking medical help due to fear of what they might discover. That’s not the case for me.
So, what exactly is healthcare anxiety?
The closest comparison I can draw is to “whitecoat syndrome,” where a person’s blood pressure spikes in response to the healthcare environment or the presence of medical professionals. Still, that’s not me. That’s not what MY anxiety is called?! Yet it’s actual, life-altering, anxiety.
My refusal to seek medical attention stems from a deep-seated lack of trust in healthcare providers. Over the years, on multiple occasions, I’ve felt neglected, disregarded, and wholeheartedly disappointed in the system, both in primary care settings and during hospital stays. The following are just a few examples but know that there are many more!
My inpatient experiences with ulcerative colitis
Hospital admission 1
During my first hospital admission for ulcerative colitis, I felt completely neglected and disregarded.
Despite undergoing surgery to remove my colon, I received inadequate care and support. Days after my surgery, I was continually ignored, all day long, when I reported my alarm at the decline in my recovery and shortness of breath. It turned out I had sepsis because the surgeon hadn’t inserted a drain (standard procedure). It wasn’t until the nurse changeover that evening, that someone actually listened. I had to have a second emergency surgery to clean me out and insert a drain. That one nurse saved my life.
I was in the hospital for almost six weeks. My mum came daily to help with personal care because it was like I was invisible to the ward nurses, and I had no idea how to advocate for myself.
J-pouch connection surgery
Another traumatic experience occurred after my J-pouch connection surgery. I was discharged prematurely, only to be readmitted shortly after due to experiencing excruciating pain, vomiting, and a distended abdomen. I was told my bowel had fallen asleep and no one could predict when it would wake up. No one communicated with me further than that or explained what post-op ileus was.
I knew nothing about inflammatory bowel disease (IBD), ulcerative colitis, or bowel surgery at that point. It was 2009, so I didn’t have the internet in my pocket, or even at home. I thought I was going to die. My mum also thought I was going to die because no one had communicated with her either. I was terrified. A few days later, I was told the scans had been reviewed again and it was post-op swelling preventing anything from passing through. I couldn’t understand how someone had misinterpreted the results. It gave me little faith in those supposedly caring for me.
Resection and j-pouch revision
Basic errors and oversights were made during my resection and j-pouch revision surgery. I endured agonising pain for hours because no one was listening to me when I said the epidural wasn’t working. It had numbed my legs and not my abdomen. Imagine feeling all of the pain of your abdomen being sliced open and intestine resected. It took 12 hours for someone to listen and remove the epidural. They switched me to a morphine Patient-controlled analgesia (PCA) machine. There had been an error in the setup, so rather than receiving morphine when I pressed the button, I was continually being administered morphine.
As you’d expect, this resulted in a morphine overdose. I remember vomiting and being in and out of consciousness. I also remember being paralysed but able to hear healthcare professionals around my bed, concerned about my shallow breathing and lack of response. They didn’t know what was wrong with me and they were fearing for my life. Of course, that meant, so was I! The next thing I remember was being shot back up to the surface when they administered naloxone.
Poor standard of care
Even standard care lacks so much. It’s Been my experience every admission, to be waiting far too long for pain relief and being majorly underdosed, making it pointless anyway. Dietary requirements are never met. And then there’s the poor quality of aftercare; disrespectful nurses, negligence etc. I can’t even count on one hand the number of times I’ve had to lay in my own faeces because they’ve ignored my buzzer. If they were busy, I could easily forgive it, but unfortunately, I have ears. I know they’re just standing around chatting at the nurse’s station rather than helping me. A patient should never feel like an inconvenience, but that’s always been my experience.
Out of the hospital
Beyond hospital settings, I’ve faced numerous challenges in receiving adequate care. Misdiagnoses, delayed referrals, and a general sense of being ignored have been constant struggles. Whether it’s being dismissed with an IBS diagnosis without as much as an examination, or enduring months of inadequate treatment for a skin condition, the healthcare system has repeatedly failed me.
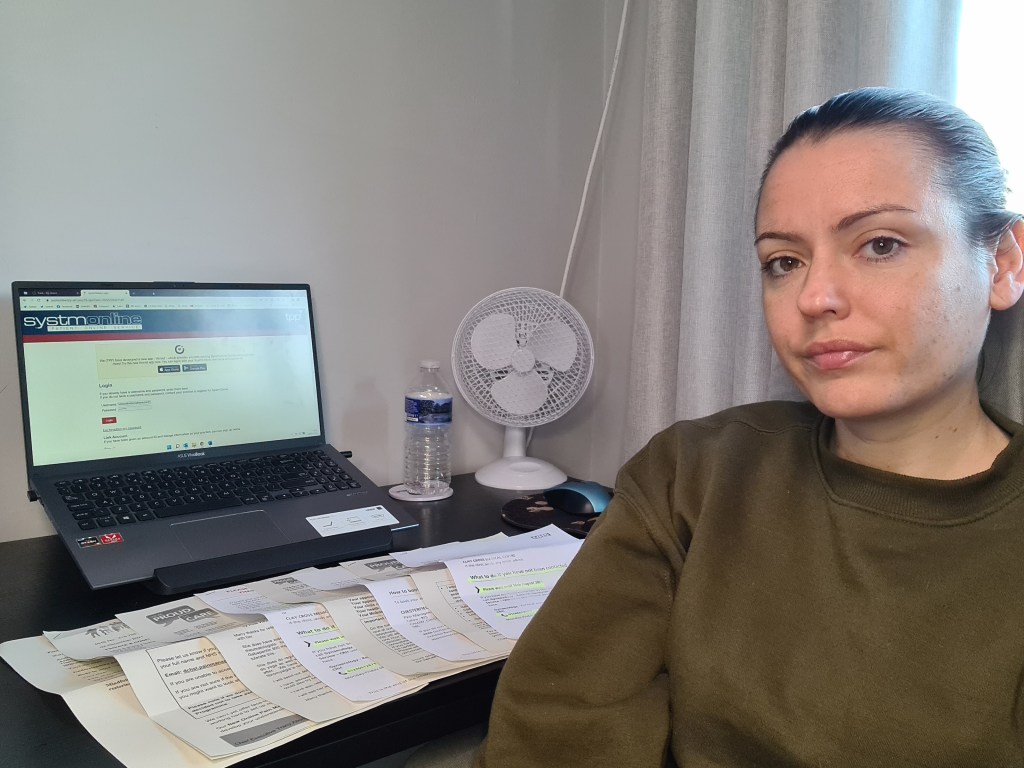
The burden of managing my health mainly falls on my shoulders. From chasing test results to ensuring referrals are processed promptly, I’ve had to become my own advocate out of necessity. Yet, even with my vigilance, mistakes and oversights persist, further eating away at my trust in the system.
This is what I call my healthcare anxiety
While I have no issue attending routine appointments or diagnostic tests, the thought of being admitted to the hospital fills me with fear and panic. Despite reassurances that it’s the best place for me, I find little comfort in the idea. I’d rather endure discomfort at home than face the uncertainty and potential neglect in a hospital setting.
I can’t really describe what happens to me when I am admitted. I have only ever been admitted for surgery because I avoid going to A&E. My heart rate goes up just thinking about it, like now. It’s as if my brain shuts down. There are no thoughts the majority of the time. I have retreated somewhere. All I can focus on is what steps I need to take to get out as fast as possible.
Smells are notorious for throwing me back into that place of anxiety. The slightest scent associated with hospitals triggers a trauma response. I have to buy different toiletries to take with me, because I know I will never be able to use them again.
I often avoid seeking medical help when I should, completely overwhelmed by the idea of having to fight to be heard. The anxiety and mental exhaustion I feel just contemplating making a GP appointment are huge. I stay home with a bowel obstruction when I know I would urge anyone else to go to the hospital. I worry that I’ll be met by someone who has no knowledge of IBD or bowel surgeries and they’ll just send me home. Then there’s the bigger fear that they might not send me home. If they don’t send me home, I’m in the hospital, which is the last place I ever want to be. This fear has continually prevented me from presenting at A&E. In fact, the last time I went to A&E was 2007, when I was diagnosed with ulcerative colitis.
In the end, my fear of being misunderstood or mistreated by healthcare professionals outweighs my fear of illness itself.
[…] the details here, but I have written about some of the failings I’ve experienced in a blog called HealthCAREanxiety, previously. Because of my experiences, I have a lot of mistrust when it comes to the healthcare […]
LikeLike
[…] blockages out at home and go through my checklist of things to help it pass. This is because I don’t trust the hospital to look after me. I’ve had too many traumatic experiences there. I know I’d tell anyone else in the same […]
LikeLike